Table of Contents
ToggleThoracic Spine Surgery: Types, Safety, Success Rates, and Recovery
When it comes to spinal health, the thoracic spine plays a crucial role in providing stability and protecting the vital organs housed within the chest cavity. In some cases, medical conditions or injuries may necessitate thoracic spine surgery. This article aims to provide comprehensive information about thoracic spine surgery, addressing concerns about its safety, various types, success rates, and recovery periods.
What is Thoracic Spine Surgery?
Thoracic spine surgery refers to surgical procedures performed on the thoracic region of the spine, which is the middle segment of the vertebral column located between the cervical (neck) and lumbar (lower back) regions. The thoracic spine consists of 12 vertebrae labeled T1 to T12, and it plays a crucial role in supporting the ribcage and protecting vital organs such as the heart and lungs.
Thoracic spine surgery may be necessary to address various conditions that affect the thoracic vertebrae, spinal cord, and surrounding structures. Some common reasons for thoracic spine surgery include Herniated Discs, Spinal Deformities, Spinal Trauma, Spinal Tumors, Degenerative Disc Disease, Spinal Infections, Thoracic Outlet Syndrome and Vertebral Fractures. Like any surgery, thoracic spine surgery involves risks and benefits. Qualified medical professionals should be consulted to make decisions about undergoing the procedure, considering a thorough evaluation of the individual’s medical history and current condition.
Is Thoracic Spine Surgery Dangerous?
One of the primary concerns patients have when considering thoracic spine surgery is its safety. It’s important to note that while any surgery carries inherent risks, advancements in medical technology and surgical techniques have significantly improved the safety of thoracic spine surgeries. Surgeons undergo extensive training and adhere to strict protocols to minimize complications.
The thoracic spine is a critical part of the spine, and any surgical intervention in this area requires careful planning, precision, and a deep understanding of spinal anatomy. Highly specialized surgeons who perform thoracic spine surgeries undergo rigorous training to develop the necessary skills for handling the intricacies of this region. Their expertise is crucial in mitigating potential risks and ensuring a successful outcome for the patient.
Surgical Advancements
Advancements in medical technology have played a pivotal role in enhancing the safety of thoracic spine surgery. Preoperative imaging techniques, such as magnetic resonance imaging (MRI) and computed tomography (CT) scans, allow surgeons to visualize the spine in great detail before the surgery even begins. This enables them to accurately identify the root cause of the spinal issue and plan the surgical approach with precision. Additionally, advanced intraoperative imaging tools, such as fluoroscopy, assist surgeons in real-time visualization during the surgery, ensuring that they can make necessary adjustments as needed.
Surgical techniques have also evolved significantly, moving towards minimally invasive approaches whenever possible. Minimally invasive procedures involve smaller incisions, reduced tissue disruption, and shorter recovery times compared to traditional open surgeries. These techniques decrease the risk of infection, reduce postoperative pain, and hasten the return to normal activities.
Patient safety is a top priority in any medical procedure, and thoracic spine surgery is no exception. Surgeons and their medical teams follow strict protocols to minimize complications. These protocols include comprehensive preoperative assessments to evaluate the patient’s overall health and identify any potential risks. Anesthesia teams tailor their approach to the patient’s medical history and condition to ensure a safe surgical experience.
Thoracic Spine Surgery Types
Anterior Thoracic Spine Surgery
Thoracic Corpectomy
Surgeons perform thoracic corpectomy, a surgical procedure, on the thoracic spine, which constitutes the middle portion of the vertebral column.The term “corpectomy” refers to the removal of a vertebral body, which is the block-like structure that makes up the front part of a vertebra. Typically, doctors use this procedure to treat conditions that cause compression or instability in the thoracic spine.
The thoracic spine comprises 12 vertebrae labeled T1 to T12, and intervertebral discs and various ligaments connect each vertebra to adjacent vertebrae.When conditions such as herniated discs, spinal tumors, severe degenerative disc disease, trauma, or spinal infections occur in the thoracic spine, they can lead to compression of the spinal cord or nerves, causing pain, weakness, numbness, and even paralysis.
A thoracic corpectomy involves removing a portion or the entirety of a vertebral body to alleviate spinal cord or nerve compression and restore stability to the spine. After removing the vertebral body, healthcare providers often fill the space with bone grafts or synthetic materials to maintain the proper spacing between the adjacent vertebrae. This helps to relieve pressure on the spinal cord and nerves while maintaining the structural integrity of the spine.
After performing a thoracic corpectomy, surgeons may need to stabilize the spine using various surgical techniques, such as spinal fusion or instrumentation (e.g., rods, screws), in order to prevent further deformity or instability.
Thoracic corpectomy is a complex surgical procedure that requires careful planning and expertise from spine surgeons. The procedure aims to relieve symptoms, improve the patient’s quality of life, and prevent neurological complications associated with spinal cord compression. Like any surgical intervention, undergoing a thoracic corpectomy entails risks and potential complications. You should make the decision after thoroughly consulting with a medical professional specializing in spine surgery.
Success Rate
Several research studies published in medical journals showcase that anterior thoracic/lumbar corpectomy and fusion surgery yield positive outcomes rated as good or excellent in over 70% of cases, addressing diverse spinal conditions.
Recovery Time
After undergoing surgery, the majority of patients experience immediate relief from intense back pain, although certain symptoms might require more time to show improvement. A recovery period of 3-7 days will be necessary, during which you will receive prescribed pain medications to ensure comfort.
Herniated Disc Thoracic Spine Surgery
Thoracic Discectomy
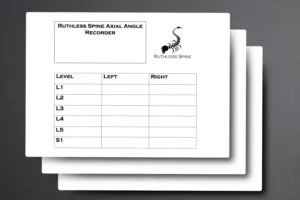
Surgeons perform thoracic discectomy, a surgical procedure, to remove damaged or herniated discs in the thoracic spine, which constitutes the middle portion of the vertebral column. The spine has distinct regions: cervical (neck), thoracic (mid-back), lumbar (lower back), and sacral (pelvic region). The thoracic spine consists of 12 vertebrae labeled as T1 to T12.
A thoracic disc herniation occurs when the gel-like center of an intervertebral disc (the soft material between adjacent vertebrae) pushes out through the tough outer layer, called the annulus fibrosus, and impinges on surrounding nerves or the spinal cord. This can lead to pain, numbness, weakness, and other neurological symptoms.
Thoracic discectomy involves making an incision in the back over the affected vertebra to access the herniated disc. The surgeon then carefully removes the portion of the disc that is causing compression on the spinal cord or nerves. Depending on the specifics of the case, surgeons may remove either the entire disc or only the herniated portion. After they remove the disc material, they may leave the space empty or fill it with a graft or spacer to help maintain the height between the vertebrae.
It’s worth noting that thoracic disc herniations are relatively rare compared to herniations in the cervical or lumbar regions. Medical professionals usually consider the surgery after attempting conservative treatments like rest, physical therapy, pain management, and other non-surgical methods, which haven’t provided sufficient relief.
As with any surgical procedure, thoracic discectomy carries risks and potential complications. These can include infection, bleeding, nerve damage, and anesthesia-related issues. Recovery and rehabilitation following the surgery can vary based on the individual patient and the extent of the procedure. It’s essential to consult with a qualified medical professional to determine if thoracic discectomy is appropriate and to understand the potential benefits and risks in your specific case.
Success Rate
In research focused on the discectomy of large transdural herniations (TDHs), it was observed that 53% of patients experienced neurological improvement, 42% remained in a stable condition, and 5% showed deterioration
Recovery Time
Recovery following minimally invasive procedures is typically significantly shorter when compared to open surgeries. The majority of patients are usually discharged on the same day as the treatment, and many can resume work within a span of two to four weeks. However, those with physically demanding occupations might need to extend this recovery period.
Minimally Invasive Thoracic Spine Surgery
Thoracic Microdiscectomy
A thoracic microdiscectomy is a surgical procedure performed on the thoracic spine (the middle portion of the spine, between the cervical and lumbar regions) to treat certain spinal conditions, such as a herniated disc or other disc-related issues. The procedure involves the removal of a portion of a herniated or damaged intervertebral disc that is pressing on spinal nerves or the spinal cord itself. The goal of the surgery is to relieve pressure on the nerves or spinal cord and alleviate associated symptoms such as pain, numbness, tingling, or weakness in the upper back, chest, abdomen, or extremities.
It’s important to note that while a thoracic microdiscectomy can be effective in relieving symptoms caused by a herniated disc, it is not always the first treatment option.
Medical professionals often attempt non-surgical approaches such as rest, physical therapy, pain management, and anti-inflammatory medications before considering surgery. Typically, patients consult with a medical professional to make the decision to undergo surgery, taking into consideration their specific condition and needs.
As with any surgical procedure, there are risks and potential complications associated with a thoracic microdiscectomy, such as infection, bleeding, nerve damage, or a recurrence of symptoms. Patients should thoroughly discuss these risks and benefits with their healthcare provider before deciding on the best course of treatment.
Success Rate
In a research study on the discectomy of large transdural herniations (TDHs), researchers observed that 53% of the patients experienced neurological improvement, 42% remained in a stable condition, and 5% saw a decline in their neurological status.
Recovery Time
The healing process following a minimally invasive procedure is typically significantly shorter when compared to open surgeries. The majority of patients can be discharged on the same day as the treatment, and many individuals are able to resume work within two to four weeks. However, those with physically demanding occupations might need to extend that recovery period.
Thoracic Endoscopic Surgery
Thoracic Endoscopic Surgery, also known as Thoracoscopic Surgery or Video-Assisted Thoracic Surgery (VATS), is a minimally invasive surgical technique used to diagnose and treat various conditions within the chest (thoracic) cavity. This approach involves the use of small incisions and specialized instruments, along with a tiny camera called an endoscope, to perform surgical procedures inside the chest without the need for large incisions or traditional open surgery.
As with any medical procedure, it’s essential to consult with a qualified medical professional to determine the most appropriate treatment approach for your specific medical condition.
Surgery performed using a tiny camera and specialized instruments through small incisions.
Success Rate
A success rate of 81% (ranging from 46% to 100%) was recorded for complete endoscopic procedures, yielding excellent to favorable results. The incidence of complications stood at 8% (ranging from 0% to 15%). Beyond detailing the sequential surgical method mentioned earlier, there are several factors that merit attention in ensuring the triumph and safety of endoscopic procedures.
Recovery Time
Recovery time after endoscopic spine surgery is generally briefer compared to traditional open spine surgery. The majority of individuals are able to resume their regular activities within a matter of days or a few weeks.
Kyphoplasty and Vertebroplasty
Both kyphoplasty and vertebroplasty are minimally invasive surgical procedures that physicians use to treat spinal fractures, particularly in the thoracic (mid-back) region. Medical professionals often perform these procedures to alleviate pain, stabilize fractured vertebrae, and improve the overall quality of life for individuals with vertebral compression fractures, which can result from conditions like osteoporosis, trauma, or cancer.
Typically, medical professionals perform both procedures under local anesthesia and guide them using imaging techniques like fluoroscopy or X-ray to ensure precise needle and cement placement. These procedures are considered minimally invasive because they involve only small incisions and do not require open surgery.
It’s important to note that these procedures are not suitable for all types of spinal fractures, and their effectiveness can vary depending on factors such as the patient’s overall health, the extent of the fracture, and the underlying cause.
Success Rate
More than 90% of individuals consider their treatment successful. Kyphoplasty has demonstrated notable efficacy in diminishing back pain and bringing about substantial enhancements in quality of life, mobility, and capacity to carry out routine daily tasks, such as walking, bending, and lifting.
Recovery Time
During the initial days after the procedure, there may be mild discomfort. However, you should be capable of returning to your regular daily routines within 2-3 days. It’s important to refrain from exertion or lifting heavy objects for a period of 4-6 weeks. Nonetheless, you’re encouraged to engage in gentle exercise and follow the specific physical therapy guidance provided by your doctor.
Thoracic Fusion and Deformity Surgery
Thoracic Fusion
Also referred to as thoracic spine fusion, surgeons use this surgical procedure to treat various conditions that affect the thoracic spine, which constitutes the middle portion of the spine located between the cervical (neck) and lumbar (lower back) regions. The procedure involves permanently connecting two or more vertebrae in the thoracic spine to stabilize the area, reduce pain, and potentially correct spinal deformities.
The procedure involves removing the intervertebral discs between the affected vertebrae and inserting bone grafts, metal plates, rods, screws, or other hardware to hold the vertebrae in place. Over time, the bone grafts will ideally fuse the vertebrae together, creating a solid, single structure. The hardware is used to maintain stability during the fusion process.
It’s important to note that thoracic fusion is a major surgery with potential risks and complications, including infection, hardware failure, and non-union (failed fusion).
Success Rate
Review of 241 thorascopic procedures showed a success rate of 98% to 100%, low morbidity, and favorable complication profile. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7671455/
Recovery Time
An analysis of 241 thoracoscopic procedures demonstrated an impressive success rate ranging from 98% to 100%. The procedures exhibited minimal morbidity and a positive profile in terms of complications.
Thoracic Spinal Deformity Surgery
Thoracic spinal deformity surgery is a surgical procedure performed to correct abnormal curvature or misalignment of the thoracic spine. Which is the middle portion of the vertebral column located between the cervical (neck) and lumbar (lower back) regions. The deformities that might necessitate such surgery include conditions like scoliosis (sideways curvature of the spine), kyphosis (excessive forward curvature, creating a hunchback appearance), and other complex spinal abnormalities.
It’s important to note that thoracic spinal deformity surgery is a complex procedure that carries certain risks and potential complications. Which can include infection, bleeding, nerve damage, and failure of the fusion process. The decision to undergo such surgery is typically made after a thorough evaluation by a team of medical professionals. The choice of surgical approach and technique will depend on the individual patient’s condition, age, overall health, and other factors.
Success Rate
Frequently encountered, the thoracic spinal fusion has a success rate ranging from 70% to 95%. Each individual patient varies, and numerous factors contribute to the overall outcome. Lumbar fusion surgery is employed to address pain situated in the lower back.
Recovery Time
Patient may resume certain restricted activities within two to four weeks. Complete recuperation usually requires a minimum of 6 to 12 months of consistent advancement.
Thoracic Tumor and Pain Management Surgery
Thoracic Tumor Resection
A surgical procedure in which a tumor located within the thoracic cavity is removed. The thoracic cavity is the space within the chest that contains vital organs such as the heart, lungs, esophagus, and major blood vessels. Tumors can develop in any of these structures. In some cases, surgical removal is necessary to treat the tumor and prevent its potential spread or further complications.
The procedure involves making an incision in the chest wall to access the tumor and surrounding structures. The size and location of the incision depend on the specific tumor’s location and characteristics. Once the tumor is accessed, the surgeon carefully removes it, along with any affected tissue or structures. In some cases, reconstruction or repair of affected organs or vessels might be necessary.
Thoracic tumor resection can be performed using traditional open surgery or minimally invasive techniques. Such as video-assisted thoracoscopic surgery (VATS) or robot-assisted surgery. Minimally invasive approaches generally involve smaller incisions and result in less pain, shorter hospital stays, and quicker recovery times compared to open surgery.
Success Rate
The general actuarial survival percentages stood at 85% after 1 year, 65% after 3 years, and 59% for durations exceeding 5 years. Correspondingly, the overall actuarial portion without any recurrence of disease was 64% at 1 year, 52% at 3 years, and 40% for periods surpassing 5 years.
Recovery Time
Feeling fatigued for a period of 6 to 8 weeks following surgery is a typical occurrence. The chest area might experience pain and swelling lasting for around 6 weeks. Sensations of discomfort or stiffness could persist for up to 3 months. Additionally, sensations of tightness, itching, numbness, or tingling around the incision made by the doctor might be felt for up to 3 months.
Thoracic Spinal Cord Stimulator Implantation
Thoracic Spinal Cord Stimulator (SCS) Implantation is a medical procedure used to manage chronic pain in the thoracic region of the spine. Chronic pain in this area can result from various conditions such as failed back surgery syndrome, complex regional pain syndrome, neuropathy, and other spinal-related issues.
The procedure involves the implantation of a small device, often referred to as a spinal cord stimulator, near the thoracic region of the spinal cord.
The way spinal cord stimulation works is by sending mild electrical currents to the spinal cord. This can interfere with the transmission of pain signals to the brain. Instead of feeling pain, the patient may experience a tingling sensation called paresthesia. This sensation can help mask or alleviate the pain, providing relief to the patient.
Before undergoing a thoracic spinal cord stimulator implantation, patients typically undergo a thorough evaluation by a pain management specialist. This evaluation helps determine whether the patient is a suitable candidate for the procedure. Also, whether previous treatments have been ineffective.
It’s important to note that while spinal cord stimulation can be effective, it may not work for everyone and results can vary. As with any medical procedure, there are potential risks and complications associated with spinal cord stimulator implantation. This includes infection, lead migration, discomfort at the implant site, and more.
Success Rate
The efficacy of spinal cord stimulators is influenced by both the specific condition being treated and the type of device utilized. On a general basis, slightly over 50% of individuals experience a pain reduction of more than 50%. It is noteworthy that the effectiveness of spinal cord stimulators might diminish over time for reasons that are presently unidentified.
Recovery Time
Ongoing Rehabilitation Following Surgery for Spinal Cord Stimulator Implantation. The majority of patients can return to their regular physical routines around 8 weeks after the surgical procedure. During the initial 6 to 9 weeks of postoperative recovery, it is advisable to modify work tasks to involve lighter duties.
Summary
In the realm of spinal health, the thoracic spine emerges as a vital stronghold, lending stability and guarding essential organs. This comprehensive article navigates the landscape of thoracic spine surgery. In itm we unravel its diverse types, addressing safety concerns, unveiling success rates, and illuminating recovery paths. From innovative imaging techniques and minimally invasive procedures to surgeries for deformities, tumors, and pain management, the intricate world of thoracic spine surgery comes to life. Surgeons’ specialized expertise, coupled with evolving technologies, fosters safer procedures, paving the way for enhanced patient outcomes and informed choices in the pursuit of spinal well-being.
Sources
- American Association of Neurological Surgeons. (n.d.). Thoracic Disc Herniation. https://www.aans.org/Patients/Neurosurgical-Conditions-and-Treatments/Thoracic-Disc-Herniation
- Mayo Clinic. (2021). Herniated Disk. https://www.mayoclinic.org/diseases-conditions/herniated-disk/symptoms-causes/syc-20354095
- Cleveland Clinic. (2021). Minimally Invasive Spine Surgery. https://my.clevelandclinic.org/health/treatments/11079-minimally-invasive-spine-surgery
- University of California, San Francisco. (n.d.). Anterior Approaches to Thoracic Spine Surgery. https://neurosurgery.ucsf.edu/conditions–procedures/anterior-approaches-to-thoracic-spine-surgery.aspx
- Spine-health. (2021). Thoracic Spine Surgery. https://www.spine-health.com/treatment/back-surgery/thoracic-spine-surgery